Kaiser Permanente research scientist and physician is helping to change the way pulmonary and critical care are provided
As a student at Harvard Medical School, Laura C. Myers, MD, MPH, found herself drawn to critical care, a field of medicine that specializes in treating people with life-threating injuries or illnesses. Physicians in this field, known as critical care specialists or intensivists, learn how to both care for patients with a wide range of medical conditions and counsel patients and family members facing difficult medical decisions.
But Myers also wanted to contribute to research that could improve the care patients in the intensive care unit (ICU) receive. So, she went on to earn a master’s degree in public health from the Harvard T.H. Chan School of Public Health and complete her clinical training with a fellowship in patient quality/safety at the Massachusetts General Hospital.
Now, as a research scientist at the Kaiser Permanente Northern California Division of Research (DOR), and a practicing intensivist for The Permanente Medical Group (TPMG) in the Diablo Service Area, covering Walnut Creek and Antioch, Myers uses the medical situations she encounters in the ICU to consider what gaps in knowledge exist and what studies might be useful in the hospital to improve patient care. We spoke with Myers, who joined DOR and TPMG shortly before the COVID-19 pandemic started, about the skillset required to work as a physician and a researcher in a learning health system like Kaiser Permanente.
What inspired you to pursue a career as a physician and researcher?
I decided to go into critical care specifically because you get to meet patients and families at a very critical moment and then guide them through a tough time. You have to gain trust very quickly and be able to explain very complicated things so that people understand how to make decisions about their loved one that makes sense for them. You often have to have difficult conversations with family members or patients when there is a poor prognosis. Being a researcher gives me another dimension to be able to think and conduct studies about how the processes of care might impact clinical outcomes. My favorite research projects are ones that are directly operationally relevant and might influence care we deliver at the bedside.
How does being part of the Division of Research and The Permanente Medical Group create research opportunities?
Kaiser Permanente is a very unique health care system. Being an embedded clinician researcher provides me opportunities to influence care delivery in ways that wouldn’t be available elsewhere. As a health system, we take care of patients both in the outpatient and inpatient setting, and thus we are able to implement programs across care settings. That is an extremely unique opportunity. While much of my research is focused on retrospective data and externally funded grants (such as from the National Institutes of Health), I also get to evaluate the impact of population-level programs implemented within our health care system. I can rigorously analyze the data, interpret it, and then help suggest operational changes to improve the way care is provided to our members. It’s a continuous cycle of learning and care improvement, where rigorous analyses can directly influence operations in the health system.

What research are you most proud of to date?
I work on a team called the Systems Research Initiative within DOR. I’m very proud of the work our team has done to develop and implement COVID-related tools during the pandemic within record time. These tools are being used by clinicians and operational leaders on a daily basis, especially during periods of inpatient surge. This work was possible because of the infrastructure we have in predictive modeling, the knowledge we have about data and data science, and the connections we have to operational leaders. Today, we are using those tools to predict COVID-19-related inpatient surges, COVID-19 related resource needs, and respiratory deterioration in COVID-19 patients.
What advice would you give medical students who are considering a career similar to yours?
Working as a researcher and a physician requires you to have a lot of different skills, so it can be quite challenging and fun. You have to master clinical work even though you’re not in the hospital every day, and you have to be able to write grants and manuscripts to be competitive in the research realm. I gained these skills in fellowship by getting an MPH degree and working directly with mentors to develop my scientific writing skills. This extra training is essential. If you are interested in health systems research, you often get your best ideas when you are in the throes of clinical care, so my advice would be to keep your eyes wide open when you’re delivering care.
What do you like to do in your free time?
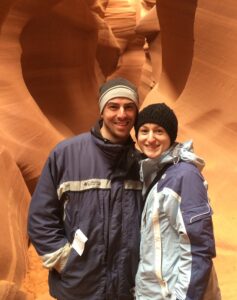
I love to hike, especially in and around the Bay Area and in national parks. My husband and I also love trying new recipes on our wood-fired grill. Before the pandemic, we loved to travel internationally, but that’s not something we’ve been able to do for a while.





This Post Has 0 Comments