Kaiser Permanente clinical trial compared methods to reach at-risk populations
Elderly Black and Latino people were more likely to get a COVID-19 vaccination after they received an email or letter from their Kaiser Permanente doctor, new research finds.
The report on the randomized clinical trial was published June 17 in JAMA Network Open.
“As the COVID-19 pandemic continues, vaccination remains the primary way for older people to protect themselves. This study provides vital information about how to reach unvaccinated older people in at-risk communities,” said study senior author Yi-Fen Irene Chen, MD, associate executive director of The Permanente Medical Group.

“This study’s randomized controlled trial design makes these findings particularly compelling. We were able to directly compare the effectiveness of different forms of outreach,” explained lead author Tracy Lieu, MD, MPH, director of the Kaiser Permanente Division of Research.
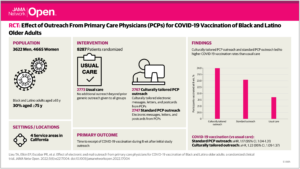
The study included 8,287 patients of Kaiser Permanente Northern California who had not been vaccinated as of March 2021 and lived in 4 communities: Central Valley, Fresno, South Sacramento, and San Jose. They were randomly assigned to 3 groups: 2,767 received culturally tailored messages about vaccination, 2,747 received standard messages, and 2,773 received no special messages beyond the usual communication about COVID-19 vaccination.
All of those in the 2 intervention groups received a vaccination message sent on behalf of their primary care physician: either an email through the Kaiser Permanente online portal or a letter in the mail if they were not signed up to use the portal. Messages were in Spanish for those who whose records said they preferred it.

The emails and letters addressed trust in the vaccines, their safety and effectiveness, side effects, and how to book a vaccine appointment. Those that were culturally tailored to Black and Latino communities also addressed issues such as cost (the vaccine is free), immigration status (vaccination is available to all and personal information is not shared with outside agencies), and racial and ethnic disparities in COVID-19 (Black/African American and Latino communities have been most harmed by the pandemic).
Four weeks later, the members in the 2 intervention groups who had not yet been vaccinated were sent a postcard that included vaccine information, a QR code, website, and phone number for booking. Those in the culturally tailored group received postcards with photos of older adults in their racial or ethnic group.
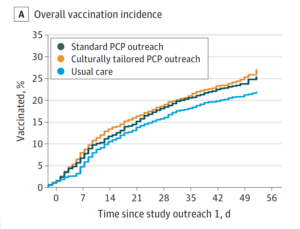
Both of the intervention groups were more likely to get vaccinated after receiving the emails, letters, and postcards, compared with the group that did not receive special communications. Eight weeks after the program’s start, vaccination rates were 24% in the culturally tailored group and 23% in the standard outreach group, compared with the usual care group that was 21.7%. The difference between the 2 intervention groups was not statistically significant.
Sending a convincing message
The study authors noted that if that 2.3% higher vaccination rate found in this study was applied to all unvaccinated Black and Latino elders in the U.S., an additional 238,000 people could have been vaccinated.
 The difference in vaccination rates was modest but larger than that seen in previous studies on vaccination outreach, the authors said. “This suggests physicians are key influencers with their patients, and outreach in the doctor’s name may be particularly effective with Black and Latino adults, who tend to have higher rates of COVID-19 vaccine hesitancy,” said Debora Sawyer, MD, an obstetrician/gynecologist with The Permanente Medical Group (TPMG) and its medical director for outpatient quality.
The difference in vaccination rates was modest but larger than that seen in previous studies on vaccination outreach, the authors said. “This suggests physicians are key influencers with their patients, and outreach in the doctor’s name may be particularly effective with Black and Latino adults, who tend to have higher rates of COVID-19 vaccine hesitancy,” said Debora Sawyer, MD, an obstetrician/gynecologist with The Permanente Medical Group (TPMG) and its medical director for outpatient quality.
As the COVID-19 vaccines were rolled out in early 2021, TPMG clinical leaders were concerned about the potential for vaccine hesitancy to limit the vaccines’ reach into at-risk communities, said Silvia Teran, MD, a TPMG physician who serves as medical director for TPMG Health Engagement Consulting Services. “The looming storm clouds were quite visible and we could see there was a disparity in vaccine acceptance,” she said. “The surveys also showed that primary care doctors rate high in trust, so we wanted to leverage that in our messaging, having it come from their doctors.”
The medical group’s patient engagement specialists researched survey data and found particular hesitancy among older Black and Latino adults, who had specific concerns about the cost of vaccination and sharing personal information with the government, such as immigration status. So those topics were addressed in the culturally tailored versions of the communications, explained Patricia Escobar, MPH, consulting manager with TPMG Health Engagement Consulting Services.
“We started out with an email to everyone in the outreach groups, which is low-cost but leaves out people who don’t use our secure messaging system online,” Escobar said. “That’s where the mailed letters and postcards come in, and we included a QR code to make it easy to access information about vaccination using their phones.”
 Teran noted the importance of working harder to reach people who don’t use technology. “There’s always that small number we can’t neglect, and often they are a higher-risk population who are older and have more illnesses,” she said.
Teran noted the importance of working harder to reach people who don’t use technology. “There’s always that small number we can’t neglect, and often they are a higher-risk population who are older and have more illnesses,” she said.
The language was designed to be encouraging but not prescriptive. One version of the postcard states, “We got the COVID-19 vaccine! Did you?” “It’s important to keep the messaging simple and direct,” Teran said.
More intensive interventions could boost vaccination rates even more than this type of targeted messaging, the authors said. These include real-time conversations, community-based outreach, and behavioral nudges, which are small suggestions meant to initiate behavior change, such as putting healthy food in easy reach.
The research was funded by a grant from The Permanente Medical Group’s Delivery Science and Applied Research Program.
Other co-authors were Nicola Klein, MD, PhD, Eric P. Elkin, MPH, Cimone Durojaiye, MPH, Stephanie Prausnitz, MS, and Charles P. Quesenberry, PhD, of the Division of Research; Nancy Goler, MD, and Stephen M. Parodi, MD, of The Permanente Medical Group; and Lucy Finn, MPH, of TPMG Consulting Services.
# # #
About the Kaiser Permanente Division of Research
The Kaiser Permanente Division of Research conducts, publishes and disseminates epidemiologic and health services research to improve the health and medical care of Kaiser Permanente members and society at large. It seeks to understand the determinants of illness and well-being, and to improve the quality and cost-effectiveness of health care. Currently, DOR’s 600-plus staff is working on more than 450 epidemiological and health services research projects. For more information, visit divisionofresearch.kaiserpermanente.org or follow us @KPDOR.




This Post Has 0 Comments