Kaiser Permanente researchers report new findings in JAMA Research Letter
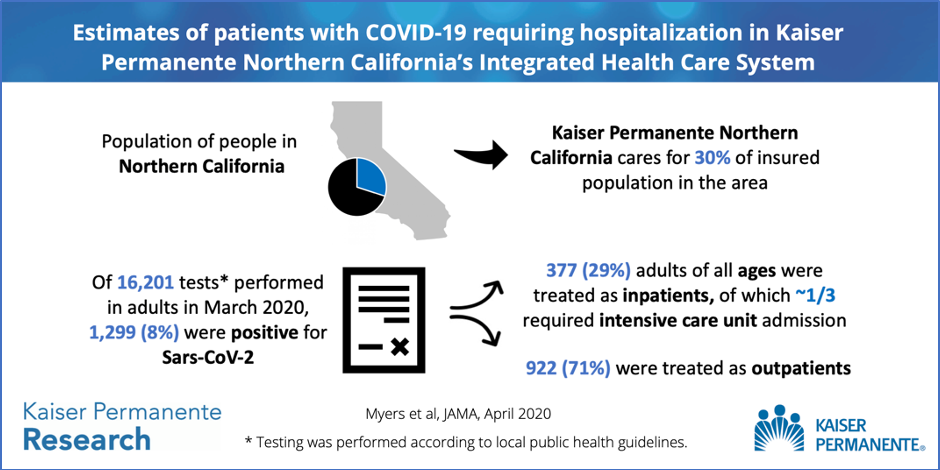
Northern California was one of the first parts of the country to experience widespread community transmission of the new coronavirus. The 4.4 million members of Kaiser Permanente Northern California make up 30% of the area’s insured population, providing a window into which individuals infected with the coronavirus require medical care. Kaiser Permanente researchers analyzed the age and health status of members admitted to the hospital and intensive care unit (ICU) with COVID-19 to learn more about the type of patients who require hospitalization. This information can help other hospitals prepare for the patients they are likely to see during this pandemic.

The new study, published April 24 in JAMA, was led by Kaiser Permanente Division of Research research scientist Laura C. Myers, MD, MPH. Coauthors include Kaiser Permanente Division of Research research scientists Gabriel Escobar, MD, and Vincent Liu, MD, and infectious disease physician and associate executive director of The Permanente Medical Group Stephen Parodi, MD. The study, which used data collected on patients hospitalized in March from all 21 Kaiser Permanente Northern California hospitals, is one of the first U.S. studies to look at overall hospital admissions. Myers and Liu talked about their study and the importance of being able to share their findings so quickly.
Q: What were the main findings?
Myers: We showed that in March 2020, 16,201 adult members of Kaiser Permanente Northern California were tested for the novel coronavirus; 1,299 (8%) tested positive. We found that 377 (29.0%) of the 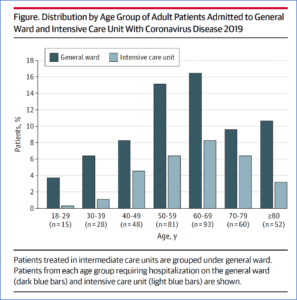 patients who tested positive needed to be hospitalized. Of these, 113 (8.7%) were treated in the ICU. Most patients treated in the ICU received mechanical ventilation. Additionally, we found that patients of all ages needed to be hospitalized for this disease, including those with few underlying health problems. Of the 377 hospitalized patients, the proportion who were age 59 or younger was similar to the proportion of adults age 60 or older. This means that public interventions to target the entire public — not just older adults — are needed.
patients who tested positive needed to be hospitalized. Of these, 113 (8.7%) were treated in the ICU. Most patients treated in the ICU received mechanical ventilation. Additionally, we found that patients of all ages needed to be hospitalized for this disease, including those with few underlying health problems. Of the 377 hospitalized patients, the proportion who were age 59 or younger was similar to the proportion of adults age 60 or older. This means that public interventions to target the entire public — not just older adults — are needed.
Q: What, if anything, surprised you?
Myers: Our results confirmed a report from the Centers for Disease Control and Prevention published in mid-March about the percentages of patients with COVID-19 requiring hospitalization and ICU admission However, our finding that 8.7% of the patients who tested positive were treated in the ICU is lower than estimates from Italy and higher than estimates from China. Since approaches to health care vary by country, it’s important to study what is happening in the U.S. so we know how to plan within our healthcare systems.
Q: How do your results add to what is known about COVID-19?

Liu: Most prior reports have focused on hospitalized or critically ill patients, which can give an incomplete perspective on an entire population. We are an integrated health care system and have access to high-quality data through KP HealthConnect, our electronic health records system, which allowed us to assess the hospitalization and ICU impact against a steady denominator. These rates are critical for surge planning and COVID-19 forecasting, and they give important anchoring data to others engaged in the fight against the disease.
Q: Why was it important to do this study?
Myers: On March 11, the World Health Organization declared COVID-19, the disease caused by the novel coronavirus SARS-CoV-2, a pandemic. As the number of cases of COVID-19 continue to grow, we feel a duty to understand this disease as quickly as possible. We felt that we could contribute to the collective understanding of the disease by publishing our early experience with percentages of patients requiring hospital and ICU level care. Journals understand the need to disseminate this important new knowledge and are processing manuscripts related to COVID-19 rapidly, especially when they have public health impact.
Q: What made it possible for you to do this study so fast?
Myers: We were able to do this study quickly because of the research infrastructure that exists within the Division of Research. Kaiser Permanente Northern California values research as an important avenue for advancing our health care organization’s mission of delivering high-quality care. Since joining Kaiser Permanente Northern California in January 2020, I have been inspired by the teamwork and collaboration I’ve seen both at the hospital and in the Division of Research. The community here has truly stepped up to deliver the best care possible for these patients despite the unprecedented level of uncertainty.
Q: What will you look at next?
Myers: We are at the very beginning of understanding this disease. In the coming months, we would like to understand what factors predict patients’ need for hospitalization and ICU admission. This would allow us to know how and when to advise patients at home to come into the emergency department and when to transfer patients from the general ward to the ICU. Having this deeper understanding should equip us to give the best advice possible for our patients.
Liu: Very few organizations can also reliably track survivors of COVID-19 hospitalization, but it’s becoming clear that there are longer-term effects of acute severe COVID-19 disease. As the country moves toward recovery, we also have to recognize the need to help individual patients and their families recover from the toll of the disease.




This Post Has 0 Comments