Kaiser Permanente study supports eventual use of test for cystatin C — instead of creatinine — to advance health equity
Editor’s note: The New England Journal of Medicine has selected this study as 1 of its 14 Notable Articles of 2021 due to its potential to change medical practice and improve patient care. The journal also highlighted the finding in a Quick Take video (free subscription required to watch).
Researchers have identified an approach to remove race from equations used to estimate a person’s kidney function. These equations have been criticized for potentially perpetuating racial health disparities. The findings, reported September 23 in the New England Journal of Medicine, are expected to inform National Kidney Foundation-American Society of Nephrology Task Force guidelines on evaluating kidney function.

“We started looking at alternative ways to measure kidney function when questions came up about whether the use of race in the equation using creatinine was actually exacerbating health disparities,” said the study’s co-senior author, Alan S. Go, MD, a senior research scientist at the Kaiser Permanente Northern California Division of Research. “Our research showed that if you use a blood cystatin C test, instead of a blood creatinine test, you don’t need to include race to get a similarly accurate estimate of kidney function.”
Creatinine is a chemical compound the muscles produce at a fairly constant rate for each person. The kidneys filter creatinine out of the blood (serum) and into urine. Testing for blood creatinine levels is the most commonly used way to measure kidney function. Since the 1990s, mathematical equations that include a person’s age, sex, and race along with their creatinine level have been used to determine estimated glomerular filtration rate, known as GFR. Age was included in the estimating equation because, on average, older people produce less creatinine than younger people. Sex was added because women typically produce less creatinine than men.
We believe that changing to the cystatin C test will promote more equity for people of all racial and ethnic backgrounds.
— Alan S. Go, MD
A controversial equation
Race — classified as Black or non-Black — was added to the equation because studies showed that, on average, creatinine levels are higher in people who are self-reported Black versus self-reported non-Black, even when kidney function is the same. Over the past year, the equation’s use of Black race has been used by reporters and activists as a prominent example of possible medical racism, and there have been calls for it to be removed.

“The recent activism has really raised the question about why we include race, here and in medicine generally, and whether we should,” said the study’s co-lead author Chi-yuan Hsu, MD, MSc, a nephrologist at the University of California, San Francisco and an adjunct investigator with the Division of Research. “There have been many calls to just take the race coefficient out of the equation. We were concerned that doing so would worsen the test’s accuracy, but we also felt it was important to move away from considering race, if possible.”
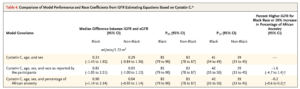
Go, Hsu, and their fellow Chronic Renal Insufficiency Cohort Study investigators looked at the impact removing race would have on the accuracy of the equations that use a creatinine blood test. They also looked at the accuracy of the equation when the degree of genetic African ancestry was substituted for race. These studies showed that independent of age, sex, and measured kidney function, Black race was associated with a 10.7% higher serum creatinine level, and that every 10% increase in genetic African ancestry was associated with a 1.3% higher creatinine result. In other words, the equation that used creatinine was more accurate if Black race or genetic ancestry was included.
“Our results show that race and genetic ancestry are linked to a person’s creatinine level, and we can’t erase that even if we account for a wide range of other factors, such as muscle mass, dietary protein intake, and other factors that are believed to influence blood creatinine level independent of kidney function,” said Go. “That math is there. So, if the purpose is to try to get the most accurate assessment of a person’s kidney function, and if you are going to rely on creatinine, then you need to incorporate Black race or genetic ancestry.”
Cystatin C allows race to be removed
But the researchers’ goal was to find a way to take race out of the equation. So, they turned their attention to cystatin C, a less-widely used test for kidney function. They found that there was no need to keep race or genetic ancestry in the equation when the cystatin C test result was put into the estimating equations. “Cystatin C solves the scientific problem of maintaining comparable accuracy and it achieves the social and scientific goal of getting rid of the need to consider race,” said Hsu.
Tests for cystatin C are currently available but they are not routinely used because the assays are not fully standardized, and they are significantly more expensive. The researchers say that if cystatin C became more widely used, the cost of the test would likely come down.
“Our work was driven by concerns raised about possible racial discrimination because Black race was taken into account in kidney function equations,” said Go. “But the equations using creatinine are also a problem because they don’t account for people of other racial and ethnic groups. Asians, Pacific Islanders and Hispanics — which are the fastest growing subgroups in this country — are all lumped into the non-Black category. Another reason to move away from using creatinine is to promote greater equity to those groups as well, and using cystatin C instead may be a way to do that.”
Funding for this study was obtained under a cooperative agreement from the National Institute of Diabetes and Digestive and Kidney Diseases. This work was also supported in part by the University of Pennsylvania; Johns Hopkins University; University of Maryland; Clinical and Translational Science Collaborative of Cleveland; University of Illinois at Chicago; Tulane University; University of California, San Francisco; and the National Center for Advancing Translational Sciences.
Co-authors include Harold I. Feldman, MD, MSCE, Wei Yang, PhD, Debbie L. Cohen, MD, Raymond R. Townsend, MD, and Jianqiao Wang of the University of Pennsylvania, Philadelphia; Rishi V. Parikh, MPH, and Thida C. Tan, MPH, of the Division of Research; Amanda H. Anderson, PhD, Jiang He, MD, PhD, and Katherine T. Mills, PhD, of Tulane University; Teresa K. Chen, MD, MHS, of Johns Hopkins University; Madhumita J. Mohanty, MD, of Wayne State University; James P. Lash, MD, and Milda R. Saunders, MD, MPH, of the University of Illinois-Chicago; Anthony N. Muiru, MD, of the University of California, San Francisco; Afshin Parsa, MD, MPH, of the National Institute of Diabetes and Digestive and Kidney Diseases; Tariq Shafi, MBBS, MHS, of the University of Mississippi Medical Center; Sushrut S. Waikar, of the Boston University School of Medicine; and Myles Wolf, MD, MMSc, of Duke University.
# # #
About the Kaiser Permanente Division of Research
The Kaiser Permanente Division of Research conducts, publishes and disseminates epidemiologic and health services research to improve the health and medical care of Kaiser Permanente members and society at large. It seeks to understand the determinants of illness and well-being, and to improve the quality and cost-effectiveness of health care. Currently, DOR’s 600-plus staff is working on more than 450 epidemiological and health services research projects. For more information, visit divisionofresearch.kaiserpermanente.org or follow us @KPDOR.





This Post Has 0 Comments