Kaiser Permanente analysis finds that early telemedicine users tended to be younger, female, and had logistical challenges to in-person visits
An analysis of over 2 million primary care appointments scheduled after the 2016 rollout of patient self-scheduling of video and phone visits at Kaiser Permanente Northern California shows that patients were more likely to choose telemedicine over an office visit if they were younger, female, or faced logistical challenges.
The study, “Patient characteristics associated with choosing a telemedicine visit vs office visit with the same primary care clinicians,” was published June 17 in JAMA Network Open.
On average, an in-person visit to the doctor’s office in the U.S. takes up 2 hours of a patient’s time. The option to schedule a phone or video appointment instead of an office visit could improve access to care. But until now, no large studies have examined the characteristics of patients who tend to choose telemedicine over in-person primary care visits within community healthcare systems.

“As video visit options expand to more patients across more medical systems, our findings lay valuable groundwork for understanding the impact of telemedicine in primary care,” said lead author Mary Reed, DrPH, a research scientist at the Kaiser Permanente Division of Research.
The authors investigated 2,178,440 primary care appointments scheduled by 1,131,722 patients at Kaiser Permanente Northern California between 2016 and mid-2018 — after patients first received the option to choose directly between scheduling video, phone, and office visits with the same primary care provider, usually their own personal doctor.
The analysis showed that in 14% of the appointments patients opted for phone or video visits instead of office visits, and 7% of the telemedicine visits were by video. Patients with the highest likelihood of choosing telemedicine were 18 to 44 years old, female, or English-speaking.
Patients were more likely to opt for telemedicine when scheduling an appointment with their usual primary care doctor. They were also more likely to choose telemedicine if they lived farther from the doctor’s office, had better access to technology, had to pay for parking at the doctor’s office, or had a higher copay for office visits.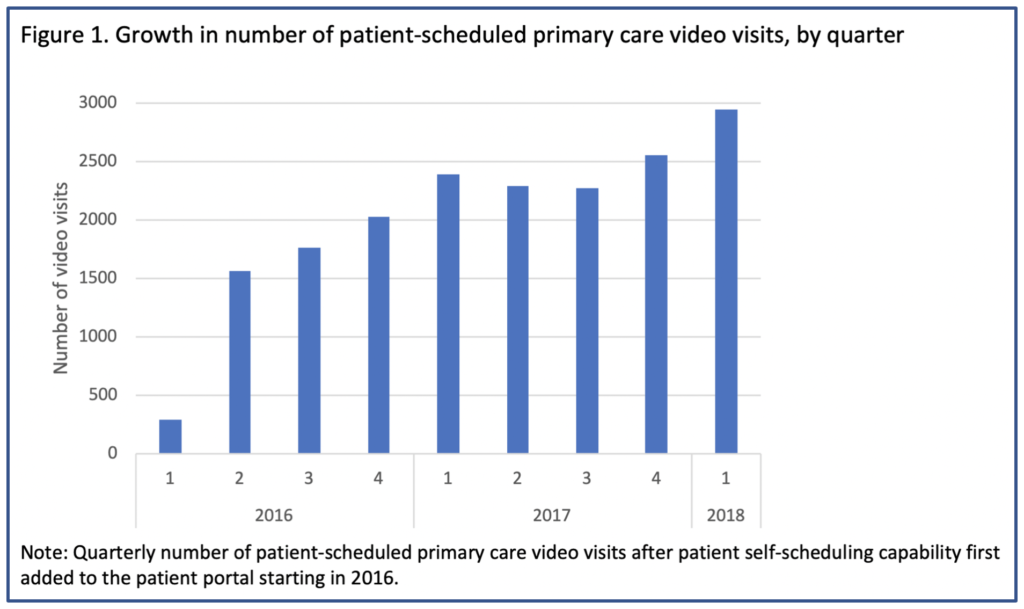
These findings suggest that telemedicine could provide opportunities to improve primary care access for people with logistical challenges to in-person visits. They also provide a foundation for comparing patient outcomes between telemedicine and office visits.
The new findings give a baseline snapshot of telemedicine choices prior to the COVID-19 pandemic. With physical distancing measures now in place, use of telemedicine has increased dramatically to make up most of the outpatient appointments at Kaiser Permanente Northern California.
“The pandemic will likely help shape telemedicine preferences in the long term,” Reed said. “Since we found that patients with prior telemedicine experience are more likely to choose it, it’s likely that our current pandemic situation could increase patients’ appetite for telemedicine going forward.”
Black or Asian patients were more likely than white patients to schedule video visits. But by far, the biggest predictor of whether a patient chose a video visit was if they had previously had one.
“This could be a sign that patients had a good experience
and wanted to use video again.” -Mary Reed
“Organizations looking to expand their use of video visits need to make it enticing for the patients to at least try video visits the first time,” said Ed Lee, MD, an internist with The Permanente Medical Group and Chief Information Officer for The Permanente Federation. “Having an experience that addresses the healthcare needs of the patient is good but creating an encounter that exceeds their expectations would help firmly establish video visits as a method of care delivery for the foreseeable future.”
Reed added, “Now that we’ve identified patient characteristics associated with choosing telemedicine, we can account for them when asking questions about outcomes, such as whether patients who chose telemedicine ended up needing more or fewer follow-up visits.”
The new study was funded by the Agency for Healthcare Research and Quality.
In addition to Reed, co-authors on the study included Jie Huang, PhD, Catherine Lee, PhD, and Chris Kennedy, MPA, of the Division of Research; Ilana Graetz, PhD, of Emory University in Atlanta, GA; and Emilie Muelly, MD, PhD, and Eileen Kim, MD, of The Permanente Medical Group.
# # #





This Post Has 0 Comments