Kaiser Permanente study used artificial intelligence to scan the electronic medical records of patients with a history of heart failure
A new Kaiser Permanente study that used artificial intelligence to scan electronic medical records found the number of patients in the hospital with worsening heart failure was 2 times higher than what was observed in primary discharge diagnoses.

“Our research shows the true burden of worsening heart failure is greatly underestimated using traditional methods,” said the study’s lead author Andrew P. Ambrosy, MD, a research scientist at the Kaiser Permanente Northern California Division of Research and a cardiologist with The Permanente Medical Group.
Physicians have speculated that reports that use primary discharge diagnoses might not comprehensively capture the number of patients hospitalized with worsening heart failure. To explore this question, Ambrosy and his colleagues turned to a type of artificial intelligence called natural language processing. They began by teaching the computer words and phrases, prescription medications, and test results found in electronic medical records that are signs and symptoms of worsening heart failure. Then, they had the computer review electronic health records for nearly 300,000 hospitalizations at Kaiser Permanente Northern California between January 2010 and December 2019 with heart failure listed as a primary or secondary discharge diagnosis.
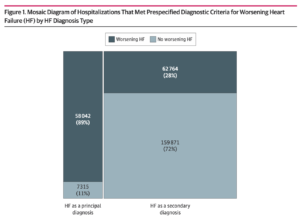
The study, published November 22 in JAMA Network Open, found that 58,042 of the 65,357 patients with a primary diagnosis of heart failure had worsening heart failure as identified by natural language processing. But among the 222,635 patients with a secondary diagnosis of heart failure, natural language processing found an additional 62,764 patients with worsening heart failure. In other words, the actual number of hospitalizations for worsening heart failure was 2 times greater than what was seen if only primary discharge diagnoses for heart failure were reviewed.
Our research shows the true burden of worsening heart failure is greatly underestimated using traditional methods.
— Andrew P. Ambrosy, MD
“Using the natural language processing creates an opportunity to identify a high-risk patient, and to do so much more accurately,” said the study’s senior author Alan S. Go, MD, a senior research scientist at the Division of Research. “You can think of it as having an expert cardiologist looking at the medical records of every patient in the hospital who has a diagnosis of heart failure. And not only can the machine work 24 hours a day, it also never gets tired of reading the notes and assessing which patients are experiencing worsening heart failure.”

Heart failure is a chronic condition that affects about 6.2 million adults in the U.S. It is one of the leading causes of illness, hospitalization, and death in older adults. Patients can be doing fine on their medications and then experience an episode when, over a few days or a few weeks, their condition worsens, and they are hospitalized for more intensive treatment. But the discharge diagnoses hospitals use do not make it easy to accurately count or identify every patient who is experiencing worsening heart failure — signs and symptoms of declining health that require a change in treatment.
The study, officially known as UTILIZE-WHF (Understanding inpaTient and outpatIent care and outcomes within a Learning and Integrated health care delivery organiZation duE to Worsening Heart Failure), is the largest-ever study to use natural language processing to home in on the experiences of hospitalized patients with heart failure.
On a patient’s medical record, “the primary discharge diagnosis is thought of as the main reason they are in the hospital,” said Ambrosy. The primary diagnosis is also used in epidemiologic studies or by hospitals to report the types of patients they are seeing with specific health issues. But it’s also possible for the main reason a patient is hospitalized to be listed as a secondary diagnosis. “This may be because the patient was hospitalized for multiple overlapping conditions,” Ambrosy said. “Or a diagnostic code that is a more descriptive term, like shortness of breath, could be the primary diagnosis while the patient’s heart failure, which was related to the shortness of breath, could be listed as a secondary discharge diagnosis.”
This more accurate assessment could help hospitals better manage their resources. But Ambrosy and Go said the goal is to do even more. “We are also interested in incorporating this technology and approach to design prospective interventions to improve care,” Ambrosy said. “We think it could also be used in our clinical trials that are looking at novel drugs and devices and care strategies to automate the process of collecting and analyzing outcomes.”
“We know that hospitalization for worsening heart failure is really a sentinel event in a patient’s history,” added Ambrosy. “It’s an important opportunity to get them plugged into our chronic care managers, consider what background medical therapies for heart failure they are on, and to determine if they need to be referred to a specialist or may need a transplant. Our work shows that natural language processing can help us identify these patients.”
The study was funded by Novartis AG.
Co-authors include Sue Hee Sung, MPH, Rishi V. Parikh, MPH, and Amanda R. Allen, BA, from the Division of Research; Anand Narayanan, MD, Rajeev Masson, MD, Phuong-Quong Lam, MD, Alan Iwahashi, MD, Kevin Kheder, MD, Alexander B. Hardwick, MD, Jesse K. Fitzpatrick, MD, Van N. Selby, MD, Harshith R. Avula, MD, MPH, and Joaquim Cristino, MSc, from The Permanente Medical Group; and Xian Shen, PhD, and Navneet Sanghera, MPharm, from Novartis Pharmaceuticals Corporation.
# # #
About the Kaiser Permanente Division of Research
The Kaiser Permanente Division of Research conducts, publishes and disseminates epidemiologic and health services research to improve the health and medical care of Kaiser Permanente members and society at large. It seeks to understand the determinants of illness and well-being, and to improve the quality and cost-effectiveness of health care. Currently, DOR’s 600-plus staff is working on more than 450 epidemiological and health services research projects. For more information, visit divisionofresearch.kaiserpermanente.org or follow us @KPDOR.




This Post Has 0 Comments