Kaiser Permanente study supports previous research showing patients avoid seeking urgent care
Emergency room physicians in Kaiser Permanente Northern California saw fewer patients with stroke symptoms at the onset of the COVID-19 pandemic than they typically do, new research shows. The study findings support previous research that suggests fear of contracting the novel coronavirus in a medical setting may have kept people from receiving critically needed medical care.
The study was published online in Stroke.
 Getting to the hospital at the first signs of a possible stroke is key to receiving effective treatment. “If someone doesn’t come to the emergency department within 24 hours of when they were last OK, they miss the window in which they might be able to have a drug that can break up the clot or have the clot removed,” said the study’s lead author Mai N. Nguyen-Huynh, MD, a research scientist at the Kaiser Permanente Northern California Division of Research and the regional director of primary stroke for The Permanente Medical Group. “We want patients to know that COVID-19 has not affected our ability to treat stroke patients quickly and that it is in their best interest to come in and be evaluated and treated right away.”
Getting to the hospital at the first signs of a possible stroke is key to receiving effective treatment. “If someone doesn’t come to the emergency department within 24 hours of when they were last OK, they miss the window in which they might be able to have a drug that can break up the clot or have the clot removed,” said the study’s lead author Mai N. Nguyen-Huynh, MD, a research scientist at the Kaiser Permanente Northern California Division of Research and the regional director of primary stroke for The Permanente Medical Group. “We want patients to know that COVID-19 has not affected our ability to treat stroke patients quickly and that it is in their best interest to come in and be evaluated and treated right away.”

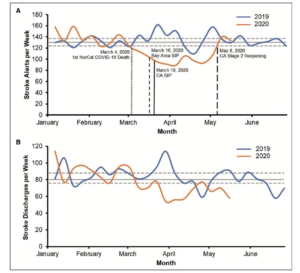
All patients who come to a Kaiser Permanente Northern California (KPNC) emergency room with stroke symptoms are evaluated by a neurologist with the KPNC Telestroke program. For the study, Nguyen-Huynh and her colleagues compared the volume of patients evaluated through the Telestroke program after shelter-in-place orders went into effect in the San Francisco Bay Area on March 16, 2020, to the volume of patients evaluated in both 2019 and the first 11 weeks of 2020. From January 2019 through December 2019, the weekly average of patients evaluated ranged from 120 to 160; from Jan. 1, 2020, to March 14, 2020, the weekly average was 136. After March 15, 2020, the weekly average dropped to 98 patients; it remained low through May 8, when California began to re-open.
The discharge rate of stroke patients also decreased after the pandemic started. “This means it wasn’t that patients with strokes just weren’t coming in within the 24-hour window,” said Nguyen-Huynh. “They weren’t coming to the hospital at all.”
The characteristics of the patients seen before and after the pandemic also differed. The 783 patients evaluated by the Telestroke program from March 15 through May 9 were more likely to have had a moderate or severe stroke score, to have a blockage in one of the major arteries in the brain, and to have been taken to the emergency room by ambulance than were the 8,337 stroke patients seen from January 2019 to March 14, 2020. The stroke patients coming to the emergency room after the pandemic started were also less likely to have other health problems.

“We thought that people with medical problems, like diabetes or lung disease, who were having stroke symptoms might have feared coming to the hospital because they had heard that people with these health problems had worse outcomes if they became infected with COVID-19,” said Nguyen-Huynh. “Our study found these people with more co-morbidities were in fact less likely to come in.”
According to the American Heart Association, more than 795,000 people in the U.S. have a stroke each year, resulting in about 150,000 deaths. About 87% of all strokes are ischemic strokes that block blood flow from getting to the brain. As a result, stroke is a leading cause of long-term disability. For Black people, the risk of having a first stroke is nearly twice as high as it is for white people. Black people also have the highest death rate due to stroke.
“It is important for individuals experiencing stroke symptoms to get to the hospital as quickly as they can,” said study co-author Stephen Sidney, MD, MPH, a senior research scientist and the director of Research Clinics at the Division of Research. “Everybody should be educated about the FAST acronym regarding stroke warning signs: F – Face Drooping, A – Arm Weakness, S – Speech Difficulty, T – Time to call 911.”
This study was supported in part by the Physician Researcher Program and the Delivery Science and Applied Research initiative of The Permanente Medical Group.
Co-authors include Xian Nan Tang, MD, PhD, Molly Burnett, MD, Jeffrey G. Klingman, MD, David R. Vinson, MD, and Alexander Flint, MD, PhD, of The Permanente Medical Group; Janet G. Alexander, MSPH, of the Division of Research; and Melissa Meighan, DNP, Kaiser Permanente Foundation Hospitals.





This Post Has 0 Comments