Joint study by Kaiser Permanente and University of Washington finds chronic kidney disease patients with implantable cardioverter defibrillators (ICDs) may not experience overall benefit
OAKLAND, Calif., February 5, 2018 — In a study of nearly 6,000 community-based patients with chronic kidney disease and heart failure, the use of implantable cardioverter defibrillators (ICDs) was associated with a significantly increased risk of subsequent hospitalization.
The study, “Long Term Outcomes Associated with Implantable Cardioverter Defibrillator in Adults with Chronic Kidney Disease,” was conducted by researchers from Kaiser Permanente and the University of Washington. It was published today in JAMA Internal Medicine.

“The finding surprised us,” said lead author Nisha Bansal, MD, MAS, of the Kidney Research Institute of University of Washington’s Division of Nephrology. “Chronic kidney disease is common in adults with heart failure, and is associated with a greater risk of heart attack. However, in this observational study we did not find a significant overall benefit from ICDs for patients with kidney disease.”
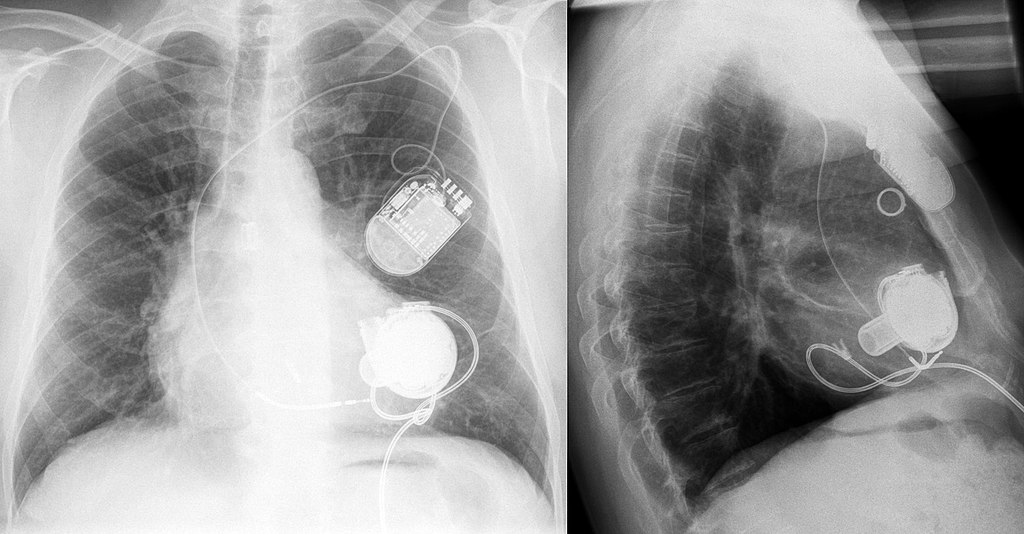
ICDs are small implantable devices that deliver electrical shocks to the heart in order to help control life-threatening irregular heartbeats, or arrhythmias. (Pacemakers are a different implanted device which gives off low-energy electrical pulses to treat less-dangerous heart rhythms.) ICDs are commonly used to try to prevent sudden death in patients at high risk of cardiac arrest.
“Because placing an ICD can be expensive and can cause other complications, it is critical to better understand how to best use this therapy in high-risk patients such as those with chronic kidney disease,” said senior author Alan S. Go, MD, a research scientist with the Kaiser Permanente Northern California Division of Research. “Based on our results, clinicians should carefully consider the risks and benefits of ICDs when recommending them for this subset of patients.”
Chronic kidney disease affects an estimated 14 percent of adults in the United States, and heart failure is the leading cause of death among them. At the same time, about 30 percent of the estimated 5.7 million U.S. adults with heart failure also have chronic kidney disease. “It’s almost a bi-directional relationship between heart disease and kidney disease,” Bansal said.
The researchers identified 5,877 adults with chronic kidney disease and heart failure with reduced left ventricular ejection fraction, all members of Kaiser Permanente’s Northern California, Southern California, Northwest and Colorado regions between 2005 and 2013; among them, 1,556 had an ICD, and 4,321 did not have an ICD.
After accounting for any differences in demographics, numerous other health conditions, the use of heart medications, and confounding risk factors, there was no difference in mortality between chronic kidney disease patients who did or did not receive an ICD. However, ICD placement was associated with a 49 percent increased risk of subsequent hospitalization due to heart failure and a 25 percent increased risk of hospitalization for any reason.
Clinical trials have examined the value of ICDs in the general heart-failure population, Go noted, and have shown that the device increases patients’ protection against sudden cardiac death and improves their overall survival. “The data from our study certainly need to be confirmed by clinical trials conducted specifically in patients with chronic kidney disease,” he added.
This study was funded the National Heart, Lung, and Blood Institute; the National Institute of Diabetes and Digestive and Kidney Diseases; and the U.S. Department of Health and Human Services.
In addition to Bansal and Go, co-authors were Adam Szpiro, PhD, and Ashveena Dighe, MPH, University of Washington, Seattle; Kristi Reynolds, PhD, MPH, Department of Research and Evaluation, Kaiser Permanente Southern California; David H. Smith, PhD, Center for Health Research, Kaiser Permanente Northwest; David J. Magid, MD, Department of Medicine, Kaiser Permanente Colorado; Jerry H. Gurwitz, MD, Meyers Primary Care Institute; Frederic Masoudi, MD, MSPH, University of Colorado Hospital; Robert T. Greenlee, PhD, Marshfield Clinic Research Foundation; and Grace Tabada, MPH, and See Hee Sung, MPH, Kaiser Permanente Northern California Division of Research.
###
To interview Dr. Bansal, please contact Brian Donohue, UW Medicine, 206.543.7856 or bdonohue@uw.edu



This Post Has 0 Comments